Signs of Nerve Damage After a Car Accident: What You Need to Know
Are you experiencing unexplained tingling, numbness, or shooting pain after your car accident? These symptoms might not be just temporary discomfort – they could be warning signs of nerve damage that require immediate medical attention.
Nerve damage from car accidents often develops gradually, making it particularly dangerous for accident victims who might dismiss early warning signs as minor injuries. Whether you're dealing with numbness after an impact injury or persistent pain in specific body areas, understanding these symptoms can make a crucial difference in your recovery journey.
This guide walks you through five critical warning signs of nerve damage after a car accident, helping you recognize when to seek medical care and what steps to take to protect your health and legal rights.
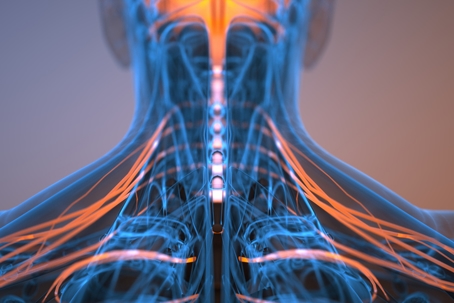
Common Impact Zones for Nerve Damage
The impact of a car accident can cause nerve damage in several critical areas of your body. Understanding these common impact zones can help you identify potential nerve injuries early and seek appropriate medical care.
Neck and shoulder nerve injuries
Your cervical spine contains eight pairs of crucial nerves that control sensation and movement in your head, neck, shoulders, and arms. During a collision, especially in rear-end impacts, the sudden jerking motion can damage these delicate nerve networks. Whiplash, one of the most frequent injuries in car accidents, can cause significant nerve compression and trauma, leading to:
- Burning sensations in your neck and shoulders
- Weakness or numbness in your arms
- Persistent headaches, especially at the base of your skull
- Reduced range of motion in your neck
Lower back nerve compression
The lower back region is particularly vulnerable during car accidents, as it bears significant force during impact. Your lumbar spine houses critical nerve networks that control movement and sensation in your lower body. When these nerves experience compression or trauma, you might experience:
The force of impact can cause herniated disks, which may compress nearby nerves, leading to sciatica - a condition causing radiating pain from your lower back down your legs. This type of nerve damage often develops gradually, making it crucial to monitor any symptoms in the days and weeks following your accident.
Extremity nerve trauma
Peripheral nerve damage in your extremities can occur through direct trauma, crushing injuries, or severe stretching during the accident. The brachial plexus - a network of nerves controlling your shoulders, arms, and hands - is particularly susceptible to injury. Similarly, the peroneal nerve in your lower leg can suffer damage, potentially causing foot drop - a condition affecting your ability to lift the front part of your foot.
If you're experiencing tingling, numbness, or unexpected weakness in your extremities after an accident, these symptoms could indicate significant nerve trauma requiring immediate medical evaluation. Remember that nerve damage symptoms may not appear immediately, and early intervention often leads to better recovery outcomes.
The Hidden Dangers of Delayed Treatment
Delaying treatment for nerve damage after a car accident can transform a potentially manageable injury into a life-altering condition. While you might be tempted to "wait and see" if symptoms improve, understanding the serious risks of postponing medical care is crucial for your recovery.
Long-term complications risks
When left untreated, nerve damage can progress into severe physical complications. Your body's natural healing process becomes compromised, potentially leading to:
- Permanent muscle weakness and atrophy
- Chronic burning or shooting pain
- Irreversible nerve deterioration
- Complex regional pain syndrome
- Coordination and balance problems
The critical window for optimal nerve recovery is typically within the first three months after injury. Beyond this point, your chances of complete recovery significantly decrease, as scar tissue develops and nerve regeneration becomes more challenging.
Impact on daily activities
Untreated nerve damage can dramatically affect your quality of life. Simple tasks you once took for granted might become increasingly difficult. Your work performance could suffer due to reduced dexterity or constant pain. Even basic activities like preparing meals, typing on a computer, or getting dressed can become challenging obstacles in your daily routine.
The physical limitations often force you to modify your lifestyle, potentially leading to reduced independence and increased reliance on others for support. This loss of autonomy can create a ripple effect, impacting both your professional and personal relationships.
Psychological effects of chronic pain
The emotional toll of chronic nerve pain shouldn't be underestimated. Up to 85% of patients with chronic pain experience depression, while anxiety affects between 30-50% of those dealing with ongoing nerve issues. You might find yourself struggling with:
Early intervention isn't just about addressing physical symptoms – it's about preventing this cascade of psychological challenges that often accompany chronic nerve damage.
Diagnostic Process and Testing
Getting an accurate diagnosis of nerve damage requires a comprehensive medical evaluation. Understanding what to expect during this process can help you feel more prepared and confident as you seek treatment.
Initial medical assessment procedures
Your diagnostic journey begins with a thorough physical examination. During this initial assessment, your healthcare provider will carefully document your symptoms and conduct a detailed neurological examination. They'll evaluate your muscle strength, reflexes, and sensory responses while asking specific questions about the accident and when your symptoms first appeared.
Modern imaging technology plays a crucial role in identifying the location and extent of nerve damage. Your healthcare team may recommend several imaging tests:
- Magnetic Resonance Imaging (MRI): Provides detailed images of nerve pathways and can identify inflammation or compression
- Ultrasound Scanning: Offers real-time visualization of nerve structures and surrounding tissues
- CT Scans: Helps identify bone-related issues that might be affecting nearby nerves
Each imaging method serves a unique purpose in creating a complete picture of your nerve injury. Your healthcare provider will select the most appropriate imaging tests based on your specific symptoms and the location of suspected nerve damage.
Nerve conduction studies explained
A nerve conduction study (NCS) is a specialized diagnostic tool that measures how effectively your nerves transmit electrical signals. During this test, small electrodes are placed on your skin to stimulate specific nerves and measure their response. This test can precisely identify where nerve damage has occurred and how severe it might be.
The test involves:
- Placing recording electrodes over your nerves
- Delivering mild electrical stimulation
- Measuring the speed and strength of nerve signals
While you might feel slight discomfort during the test, it's generally well-tolerated and provides valuable information about your nerve function. Combined with EMG (electromyography), these studies help your healthcare team develop a targeted treatment plan for your specific type of nerve damage.
Remember, early diagnosis through these comprehensive testing methods significantly improves your chances of successful treatment and recovery. Your healthcare provider will guide you through each step, ensuring you understand the purpose and importance of each diagnostic procedure.
Recovery Timeline and Management
Understanding your recovery timeline after nerve damage can help set realistic expectations for your healing journey. While each case is unique, knowing what to expect can help you stay focused on your recovery goals.
Short-term vs long-term recovery expectations
Your nerve recovery process typically spans several stages. During the first 3-4 weeks, you'll focus on managing inflammation and protecting the injured area. The next 3-6 months are crucial for nerve regeneration, though complete healing may take up to two years in severe cases. Remember that age plays a significant role in recovery speed, accounting for up to 50% of the variance in success rates.
Physical therapy and rehabilitation options
Physical therapy serves as a cornerstone of your recovery process, offering several key benefits:
- Restoration of mobility and strength
- Prevention of muscle atrophy
- Customized exercise programs
- Improved circulation for better healing
Your physical therapist will create an individualized treatment plan based on your specific injuries and recovery goals. Early intervention through physical therapy can significantly enhance your recovery prospects and help prevent long-term complications.
Managing your pain effectively requires a multi-faceted approach. Short-term strategies include rest, ice therapy, and over-the-counter anti-inflammatory medications. For longer-term relief, your healthcare provider might recommend:
Prescription medications targeting nerve pain Alternative therapies such as acupuncture or massage Cognitive-behavioral therapy to address psychological aspects of chronic pain
Remember that pain management isn't just about medication – it's about finding the right combination of treatments that work for you. Your healthcare team will adjust your pain management strategy as you progress through different stages of recovery, ensuring you receive appropriate support throughout your healing journey.
Conclusion
Nerve damage after a car accident requires quick action and proper medical attention for the best recovery outcomes. Your symptoms might seem minor at first, but waiting to seek treatment could lead to permanent nerve damage, chronic pain, and significant lifestyle changes.
Medical documentation from early diagnosis and treatment strengthens your position when seeking compensation for your injuries. Each diagnostic test and therapy session builds evidence of your injury's severity and necessary recovery costs.
Remember that nerve damage recovery takes time and patience. While some cases heal within months, others might require up to two years of dedicated treatment and rehabilitation. Stay committed to your treatment plan, work closely with your healthcare team, and give your body the time it needs to heal properly. Your diligence now can prevent complications and support optimal recovery later.